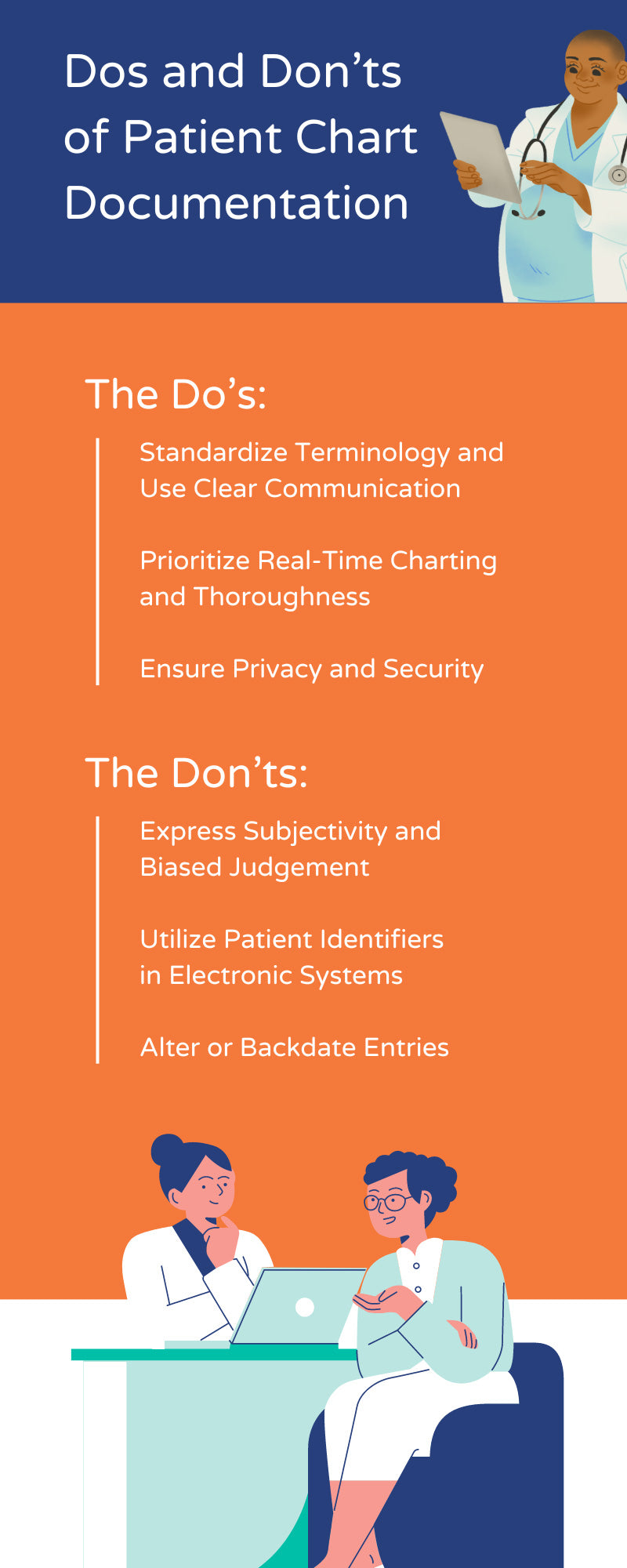
Effective patient chart documentation is not just about penning down notes—it's an art and a science that directly influences the quality of patient care. As healthcare providers, your meticulous documentation is the backbone of efficient and effective healthcare, underscoring the importance of your role in patient recovery, medical office efficiency, and legal protection.
The efficiency of your documentation is essential to your workflow and the health of your patients. Let’s explore the minutiae of patient documentation, highlighting the nuanced dos and don'ts of patient chart documentation from seasoned practitioners to fresh-faced medical students who must know this information by heart.
Telling a Patient's Story
Patient documentation is the narrative that tells the story of a healthcare encounter—the patient's ailments, the treatments administered, and the prognosis. When done right, it paves a clear path toward patient recovery and ensures the profound trust that patients bestow upon their healthcare guardians. But when documentation is lacking, inconsistent, or rife with errors, the repercussions can be dire.
The Dos of Patient Chart Documentation
Effective patient chart documentation is a critical skill that requires meticulous attention to detail and a deep understanding of clinical narratives. It serves as the foundation upon which accurate diagnoses, treatment plans, and patient safety measures are built.
In the following section, we highlight the key things to remember for patient documentation, emphasizing practices to adopt for the creation of secure and highly accurate patient records.
Standardize Terminology and Use Clear Communication
Using standardized terminology is not just a preference; it's a necessity. Utilizing clear, consistent, and universally understood language in your documentation empowers all caregivers, from seasoned practitioners to fresh-faced medical students, to interpret the chart accurately. This not only streamlines communication within the healthcare team but also respects the patient's story with precision and a universal standard, thereby improving the quality of your documentation.
Prioritize Real-Time Charting and Thoroughness
There's no room for procrastination in charting. The moment an assessment is made or treatment is given, that data should be input into the patient's record. This fast approach doesn't compromise the quality of notes—it ensures nothing falls through the cracks. Real-time charting is a comprehensive snapshot, a point-in-time look at the patient's state and the care provided, leaving no detail overlooked.
Ensure Privacy and Security
Protecting patient data is non-negotiable. Every scribble, click, and keystroke that makes it into a chart holds sensitive information, information that should be guarded more fiercely than gold. Adhering to regulations such as HIPAA means understanding that patient privacy is a fundamental right and integrating practices that secure it without fail.
The Don’ts of Patient Chart Documentation
Navigating the complexities of patient chart documentation requires vigilance to avoid common pitfalls. It's critical to stay informed about the practices that could potentially compromise the integrity or utility of patient records. Avoiding certain habits can ensure the most accurate and secure patient records possible.
Express Subjectivity and Biased Judgement
Assessments should be based on evidence, not on the feeble grounds of personal bias or opinion. Healthcare providers should chart what they see, hear, feel, and measure. This way, patients can get an unbiased and accurate diagnosis.
Utilize Patient Identifiers in Electronic Systems
Even with stringent security protocols, the use of patient identifiers in electronic systems can be an Achilles' heel for data breaches. Instead, utilize patient identifiers internally. This helps protect patient privacy while maintaining the link between medical records and an individual.
Alter or Backdate Entries
Once made, entries should not be backdated or changed unless a legitimate error has been identified and a proper correction is completed. This can be achieved by accurately identifying and amending the mistakes, ensuring the final output adheres to the highest standards of accuracy and clarity. Intentional alterations can lead to devastating consequences, legally and ethically.
The Impact of Good Documentation on Patient Care and Legal Protection
Good documentation serves as a compass for patient care, leading healthcare providers down a well-informed, evidence-based path. It guides decision-making, ensures continuity in care, and offers a solid foundation for effective communication among care teams and across different healthcare settings.
In a legal sense, precision in charting can be the difference between innocence and guilt. In the event of a malpractice claim, the one thing that speaks louder than the provider's words is the patient's chart. It's a time-stamped record that, if maintained correctly, can exonerate the provider from false claims or uncertainty.
Best Practices for Teaching and Implementing Good Documentation Habits
The foundation of superior patient care and legal safeguarding is no doubt rooted in the meticulous practice of accurate chart documentation. However, the path to excellence is not solely the responsibility of individual healthcare providers; it also hinges on a collective effort to foster an environment conducive to learning and adherence to best practices.
Let's explore three crucial habits that, if adopted in healthcare environments, can significantly improve the quality of patient chart documentation.
Continuous Training and Education
Charting isn't a static skill. It evolves with medical knowledge, technology, and regulatory changes. Continuous education equips healthcare providers with the latest standards and best practices. Ongoing training through workshops, webinars, and institutional protocols is the key to accurate documentation.
Supervised Practice and Feedback Loops
The best education is experiential, and for documentation, that means practice. Regular audits and feedback loops provide invaluable experience and instantaneous corrections. This not only hones the skills of new providers but also refreshes the skills of seasoned professionals.
Technological Assistance Without Over-Reliance
Charting technologies are marvels of modern healthcare, but they should act as tools, not crutches. Providers should leverage these advancements to enhance their documentation procedures, not replace them. Understanding the capabilities and limitations of technology is fundamental to maintaining a balance where documentation remains both technologically advanced and ethically sound.
Precision is paramount. Each charted encounter is an endeavor to provide the best possible care under the watchful eye of the law and with unfaltering respect for patient privacy. By adhering to the dos and don’ts of patient chart documentation, healthcare providers not only fortify the quality of care they provide but also safeguard the trust and well-being of their patients.
At Carstens, we understand the critical role of documentation in healthcare. That's why we're not just suppliers of medical office supplies; we're advocates for seamless and thoughtful charting practices that elevate patient care. Together, we can empower the healthcare community to chart with clarity, compassion, and precision.